MODULE 23 short answer questions
saq 1.
A 6 month old baby is brought in by his mother and father. They are concerned because he has had a period of unresponsiveness after feeding.
Question 1. (6 marks)
What features will you ask about on history in each of the following categories?
presenting complaint (2 marks)
Question 2. (2 marks)
Give 2 bedside investigations you will perform.
Must include:
Question 3. (5 marks)
Define the term “apparent life threatening event”.
Must include:
non specific diagnosis but includes any event frightening to child’s carer
And includes one or more of: (1 marks each)
Question 1. (6 marks)
What features will you ask about on history in each of the following categories?
presenting complaint (2 marks)
- details of what happened such as apnoea/cyanosis/coughing
- intercurrent infective Sx
- birth history and gestation
- development, particularly weight
- immunizations
- intercurrent medical conditions (esp cardiac/respiratory)
Question 2. (2 marks)
Give 2 bedside investigations you will perform.
Must include:
- BSL
- ECG
Question 3. (5 marks)
Define the term “apparent life threatening event”.
Must include:
non specific diagnosis but includes any event frightening to child’s carer
And includes one or more of: (1 marks each)
- Apnoea
- Colour Change
- Abnormality of muscle tone
- Choking or gagging.
saq 2.
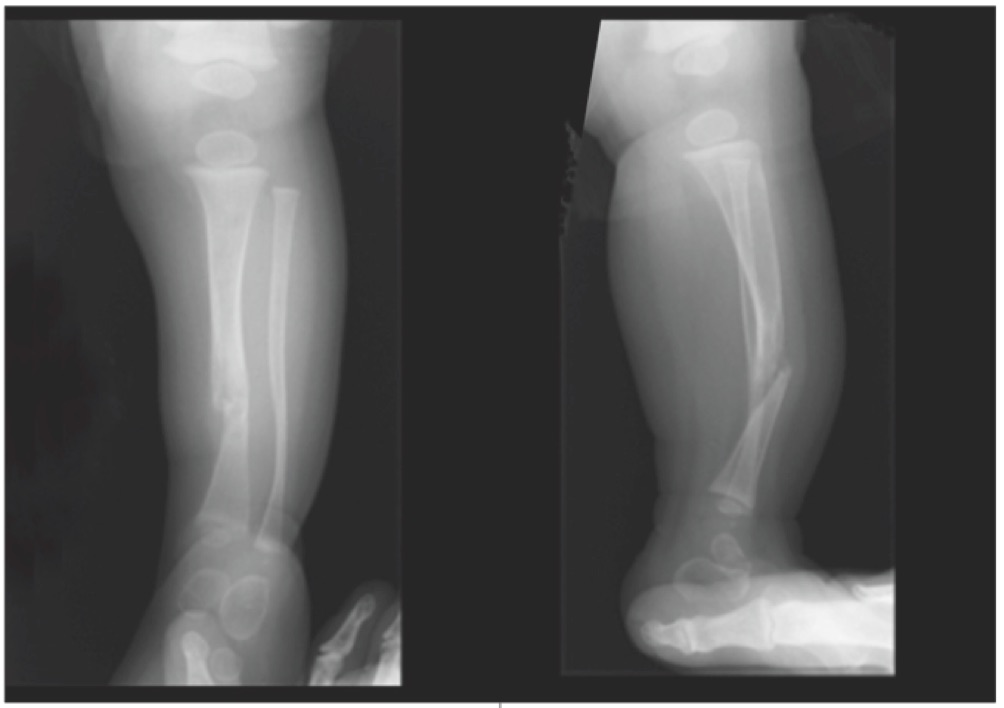
An 11 month old boy is brought in by his grandmother with leg pain. The resident has ordered an xray, and the images are shown below.
Question 1. (2 marks)
What does the image show?
Must include:
Question 2. (2 marks)
What are the implications of this injury?
Must include:
Question 3.
Under the headings below outline how will you manage each element of this situation?
Child (3 marks)
Grandmother (3 marks)
Consultations (2 marks)
What does the image show?
Must include:
- comminuted midshaft tibial fracture (1 mark) with dorsal angulation of the distal tibia (1 mark)
Question 2. (2 marks)
What are the implications of this injury?
Must include:
- in a premobile child strongly suggests non accidental injury.
Question 3.
Under the headings below outline how will you manage each element of this situation?
Child (3 marks)
- analgesia that is appropriate: eg fentanyl 2ug/kg of IN fentanyl
- immobilize limb in cast
- evaluate for other injuries
Grandmother (3 marks)
- open disclosure of diagnosis and concerns
- explanation of actions, centred on welfare of child
- clear documentation of all assessment/action taken
Consultations (2 marks)
- orthopaedic surgeons
- child protection unit
saq 3.
A 6 year old boy with a history of asthma presents with his parents. They state that his asthma is “playing up”. He has a history of previous ICU admissions with his asthma.
Question 1. (6 marks)
Give 6 features on examination you will assess for in this child?
Must include:
Question 2. (2 marks)
The child is using accessory muscles, has oxygen saturations of 91% on RA and a respiratory rate of 61. On ascultation there is no wheeze and minimal air entry bilaterally. How would you grade the severity of this child’s asthma?
Must include:
life threatening
Question 3. (4 marks)
The child weighs 21kg. What initial treatments will you institute?
Must include:
Question 4. (2 marks)
The child is not responding to your initial treatment, and escalation is required. What treatments will you administer now?
Must include:
IV salbutamol 5mcg/kg.min = 100mcg/min titrated downwards
Use of CPAP 5cm H2O if available/institute high flow oxygen.
Question 1. (6 marks)
Give 6 features on examination you will assess for in this child?
Must include:
- Respiratory rate
- Oxygen saturations
- Respiratory effort: use of accessory muscles
- Presence of cyanosis
- Ability to speak
- Degree of wheeze on ascultation
Question 2. (2 marks)
The child is using accessory muscles, has oxygen saturations of 91% on RA and a respiratory rate of 61. On ascultation there is no wheeze and minimal air entry bilaterally. How would you grade the severity of this child’s asthma?
Must include:
life threatening
Question 3. (4 marks)
The child weighs 21kg. What initial treatments will you institute?
Must include:
- continuous nebulised salbutamol (1 mark)
- oxygen for sats >95%
- ipratropium 500ug x 3 nebs over 60 minutes
- IV MgSO4 5-10 mmol IV over 20-30 minutes
- IV hydrocortisone 50-100mg
Question 4. (2 marks)
The child is not responding to your initial treatment, and escalation is required. What treatments will you administer now?
Must include:
IV salbutamol 5mcg/kg.min = 100mcg/min titrated downwards
Use of CPAP 5cm H2O if available/institute high flow oxygen.
saq 4.
A 2 year old boy attends ED with his parents, who are concerned that he has had a fever for the past twelve hours. The child is normally well and has no relevant medical history of note. He has a fever of 38.2 oC.
Question 1. (4 marks)
Give 4 clinical signs that would indicate that this child is toxic?
Must include 3 out of 4:
Question 2. (2 marks)
The child has no signs of toxicity, but has vomited twice and appears mildly dehydrated. How would you perform a trial of fluid?
Must have a reasonable description of TOF incorporating:
Question 3. (2 marks)
What investigations will you perform (if any) in this child?
Must include
Question 4. (6 marks)
The parents have read on the internet about Kawasaki disease. What are the diagnostic criteria?
Must include:
Question 1. (4 marks)
Give 4 clinical signs that would indicate that this child is toxic?
Must include 3 out of 4:
- altered level of consciousness
- increased work or rate of breathing
- altered colour: pale/mottled or prolonged capillary refill
- significantly decreased urine output/significant dehydration on exam.
Question 2. (2 marks)
The child has no signs of toxicity, but has vomited twice and appears mildly dehydrated. How would you perform a trial of fluid?
Must have a reasonable description of TOF incorporating:
- 0.5ml oral rehydration solution/kg every 5-10 minutes
- administered by parent, and recorded by same
Question 3. (2 marks)
What investigations will you perform (if any) in this child?
Must include
- BSL
- Urinalysis
Question 4. (6 marks)
The parents have read on the internet about Kawasaki disease. What are the diagnostic criteria?
Must include:
- >5 days of fever plus:
- conjunctival injection
- polymorphous rash
- mucous membrane inflammation/strawberry tongue
- desquamation of the hands/feet
- cervical lymphadenopathy
SAQ 5.
Compare and contrast Measles and German Measles using the table below. (10 marks)
|
ITEM
causative agent incubation period method of transmission Fever prodromal features nature of rash onset & duration of rash sequelae |
MEASLES
Measles (rubeola) virus (RNA Morbillivirus) 7 - 14 days respiratory/droplet High (>38.5oC) (4 - 7 days prior to rash) cough, conjunctivitis and coryza koplik spots maculopapular erythema, darkens as progresses 7 days post cough, lasts 3-4 days immunosuppression with bacterial pneumonia and otitis media |
GERMAN MEASLES
Rubella virus (RNA, Rubivirus) 14 - 21 days respiratory/droplet Low (<38.5oC) (1-5 days prior to rash non specific Sx (sore throat/headache etc) pink maculopapular rash lighter than measles 1-5 days post prodrome, rash completely resolved within 3 days congenital rubella Sx in pregnant women |