|
How to pass the Fellowship MCQ Exam. That's the question on everyones lips as we head towards the pointy end of studying for the exam.
If you have never sat this exam before, let me tell you, the ACEM Fellowship exam, is a long day, so be rested. 3 hours of SAQ exam and 3 hours of MCQ/EMQ exam. You need to be able to think. Here is some simple exam strategy for the MCQ. This is revision for all the Fellowship Exam Course candidates, but important to remember.
Create a 'Hard Facts' File, where you keep the facts you need to have for the exam. Peter Kas
0 Comments
I had a very good question from one of our students, and I've reproduced it here for people to think about..... The question was : should we expect a question on TEG or ROTEM in the exam? "..studying smart - the important things that are likely to be on the exam..." Three times in every six month course we send out formal exams to our students. Each of them provides valuable feedback in terms of exam technique.
Every year, I give my predictions of the top questions for the Fellowship Exam. Usually, my hit rate is good. One of my students recently said, "I should have just studied your top 30 list". I don't recommend this, but here is another year's predictions.
The predictions are based on:
When you understand the above behaviours, the chances drop significantly. Although I do give all my guys in the Fellowship Course the top 30, the list I'll give here is: "You're Crazy If You Don't Know these Seven" 1. ECG: MOBITZ BLOCKS The Mobitz block is one of the most popular questions in the exam and a sure bet. In fact two ECG's are a sure bet. Any person with syncope and an ECG, remember the 'ECG's of Syncope'. Beware the hidden p waves. Understand the significance of clumping of QRS's Know the importance of the p-p interval. Try some examples 2. FLUID MANAGEMENT IN CHILDREN Understanding fluid resuscitation in children has become very popular recently. Nowhere moreso than in the area of DKA in children. The fear ( regardless of some saying it is irrational) of cerebral oedema in children has resulted in some states producing specific Emergency Department Guidelines for the management of DKA. For a quick review complete the module DKA in Children. 3. SEIZURES IN CHILDREN This is always a good area. The progression down the seizure algorithm, the knowledge of the various drugs and the ability to know when and how to secure the airway make this an area that is 'choc full of goodness' for the examiners. Certainly some areas, such as airway are more suited to the OSCE, however this kind of question suits both. 4. TRAUMA Trauma is one of the major areas in the Emergency syllabus. Although the big topics such as chest trauma and management of the unstable pelvic fracture are great exam questions, I think its also important to look at the slightly smaller stuff. Burns have been asked before, however electrical burns are a great topic. An understanding of the difference in AC versus DC current, the different types of burns including, flash, arc and thermal burns, as well as the futility of the Parkland Formula for fluid resuscitation, in these presentations, makes this a great area to draw questions from. 5. ANYTHING TO DO WITH EYES The examiners have a long standing love affair with the eye and repeat the questions often. I suppose that this is because they make great pictures. This about all the different conditions they can ask:
6. ANYTHING TO DO WITH THE NECK Just when we think, we've done the neck and we won't get that any more, we get the neck again. Why? It can represent a true emergency and it make a great picture. This can be abrasions, penetrating injury or lacerations. 7. THE BLOOD GAS This has been, is and will always be a favourite. If you've done the Fellowship Course or The ABG MODULE here on Resus if you've read Luke Lawton's great book 'Own The ABG', with example after example to practice on, you know just how simple interpreting the ABG/VBG can be. Get ready for the triple abnormality; look for it. Know the cause of more than RAGMA. Know the NAGMA. If they give an osmolality, its almost alway going to be an alcohol issue. Ok there you go. There are no surprises there I hope. This is 'bread and butter' stuff. Good luck in the exam. See you at the Course and see you as FACEMs soon. Peter Kas CEREBRAL OEDEMA IN DKA: DO WE REALLY KNOW THE CAUSE?
We recently had a child with DKA in our department and the subject of fluid resuscitation came up. Also the Queensland Government guidelines on the Emergency Management of children with DKA has recently been produced. I thought it was timely to revisit a blog I wrote in 2014 on the evidence on this topic, as well as set up a teaching module on DKA ( more on this at the end) Cerebral oedema is the most feared complication in children presenting with Diabetic Ketoacidosis (DKA). It occurs in about 1% of cases but has a mortality rate of up to 90% (Waldorf J et al Diabetes Care 2006; 29:1150-9). Patients will have a decreased conscious state and may also have cranial nerve palsies, headache and/or bradycardia and hypertension. Its incidence has remained the same since it was described in 1936 and although we have clues as to what may contribute to it, and we know that some patients have subclinical cerebral oedema even at presentation(Krane et al NEJM 1985;312:1147-51), we still can't predict who will get it, nor greatly affect its high rate of mortality. There are theories of causative factors, most of which are vasogenic or osmotically based, but the studies are small or retrospective, or both. WHAT CAUSES IT? - THEORETICALLY One theory relates to osmolytes accumulating in brain cells. These are the compounds that maintain normal cell volumes. As extracellular osmolality decreases rapidly with treatment, water flows rapidly onto these cells causing the brain to swell. Another theory relates to Na+ / H+ exchanger, such that a correction of acidosis results in Na and water passing onto the brain cells, resulting in oedema. WHAT CAUSES IT? - IN PRACTICAL TERMS We believe that the following increase the chance of developing cerebral oedema: 1 Newly diagnosed diabetes 2 Duration of symptoms 3 Rapid change in Osmolality (2xNa + U + Glc): i.e., a rapid decrease in Glucose and a decrease in Sodium 4 Initial pH < 7.1 ................ and in more recent studies (Glaser N et al NEJM 2001;344:264-269) 5 Decrease in CO2 6 Increased Urea 7 If treated with Bicarbonate WHAT DOES THIS MEAN IN TERMS OF TREATMENT? FLUIDS: If the patient is hypotensive and crashing then fluid resuscitation is necessary. No question about it. However, how much we give may matter. In some of the work published there is an indication that more than 40ml/kg given over the first 4 hours may predispose to cerebral oedema. We seem to be conditioned to give 20ml/kg to every child. My approach is a little less aggressive. I aim at 5ml/kg if the child is very unwell and crashing. I then review and give it a little time ( that may only be minutes) before more fluids are given. The point is, unless the child is crashing we don't have to give large volumes, we can pull back a little. The recommendations look at tolerating a systolic blood pressure of (70 + 2 x age)mmHg. We must remember that kids don’t have much room, when they decompensate and that hypotension is a late sign. However it is this very group of children that we may be harming. If the blood pressure is OK, leave them be. If you really have to give fluids ( because it is so conditioned that its an automatic reflex), give 1ml/kg and wait. The usual approach to fluids is to calculate the deficit and ongoing maintenance needs and give over 48 hours. INSULIN AND GLUCOSE LEVELS: Large rapid drops in glucose, or a rapid decrease in osmolality can, according to the osmotic theory, cause cerebral oedema. Hoorn et al (J pediatr 2007:150: 467-473), found that a drop in osmolality from 304 + 5 to 290 + 5, was associated with increased cerebral oedema. WHAT SHOULD WE TAKE AWAY FROM ALL OF THIS AND WHAT SHOULD WE DO? The evidence isn't great. What we see is that the more acidotic you are, the more deranged your electrolytes, the more abnormal your physiology, the worst you do. The sicker kids did badly. Common sense. Firstly it's important to say that it's very rare that you will see one of these cases unless you are working in an ED that sees lots of kids. That's why its even more important to know what to do, because its not that frequent. If a child is sick and haemodynamically crashing, then give fluids. I don't give 20ml/kg of normal saline right away. I will give 5-10ml/kg and then review. I can always give more if needed. I don't give a bolus of insulin, I start an infusion(after fluids are initiated and probably not before 1-2 hours) and wait for gentle lowering of the blood sugar i.e.., < 5mmol/L drop per hour. Things improve over hours. Nothing needs to happen quickly here. If I think a child has cerebral oedema, mannitol 1g/kg IV is the treatment of choice. You must discuss these patients with endocrine/Paediatrics and ICU. If the conscious state deteriorates to the point where protection of the airway is needed, or if airway control is necessary to paralyse and lower intracranial pressure( if this indeed assists in this case), then beware not to hyperventilate the patient. Hypocapnia from mechanical ventilation has been associated with this condition(Glaser N et al NENM 2001;344:264-269) Cerebral oedema, if it occurs, is a difficult condition to treat and the outcomes aren't good. We don't really know if our treatment contributes to the development. However, we need to do everything we can, to ensure it doesn't. Click below to complete a real time case module online, that will help reinforce the management of DKA. Hello to all of you planning to sit the Fellowship Exam in August.
This is a critical time for your preparation. This is about the time that you get sick of it and don't want to continue. You say "I've had enough and won't do this any more. I'll just locum for the rest of my life!" You and I know its not true. You need a couple of days off before you begin again. Take a few days and just study one topic. Plan to be an expert in that topic i.e.., hypothermia. The key is to give yourself a break, but to also study a potentially high yield topic. As you get closer to the exam and at about this time, I put together what I think may be a list of topics that will appear. For those that have done the Fellowship Course in the past, my strike rate is between 30% and 50%. How to approach this list: Don't just study this list! Study as you normally do, however spend a little more time on these topics. What are they? For those of you doing the Fellowship Course, They will come out next week, on that week's resource page. Enjoy and good luck! The New Atach-2 trial is out- what did they find in terms of bp control in intracranial bleeds?18/6/2016 Two days after speaking at the EMCORE Conference on blood pressure control in intra-cerebral bleeds the ATACH-2 trial (Antihypertensive Treatment of Acute Cerebral Haemorrhage II) has been published.
We know that intra-cerebral bleeds are dynamic, with up to 40% of patients having growth in haemorrhage volume, in the first 3 hours(Stroke 1997:28:1-5). We also know that bleed volume is a determinant of mortality and that bleed volume increase, is related to increased blood pressure(Neurosurgery 1994). Because of this, there has been a push to lower systolic blood pressure(SBP) in acute bleeds. I am not including subarachnoid bleeds in this discussion. I recently wrote a blog titled the ‘Penumbra Conundrum‘ and pointed out that hemorrhagic strokes are very different to ischaemic strokes. Hemorrhagic strokes have no ischaemic penumbra around the haematoma. Cerebral blood flow slows in the region as does metabolic rate (Stroke 2013:44;620-6). The INTERACT 2 trial(NEJM 2013: 368: 2355-2365) randomised over 2000 patients into two systolic blood pressure groups:
The original ATACH-I trial used Nicardipine to lower SBP safely down to 110-140 (Crit Care Med 2010;38:637-648). The ATACH-II Trial just released, was a randomised multi centre trial that recruited patientswithin 4.5 hours of symptom onset. The blood pressures were kept at one of two levels for 24 hours:
1000 patients were randomised equally into the two groups. The study was stopped early, short of its 1280 patient target, due to futility. There was no difference in survival or benefit between the 2 groups i.e.., the intense lowering of SBP group and the less aggressive group. There may have been some increase in renal adverse events (not statistically significant) in the first 7 days in the more aggressive group, however the clinical implications of these are unclear. Both INTERACT -II and ATACH-II show no benefit in lowering blood pressure in intra-cerebral bleeds. So where to now? What about the patient with SBP of 220mmHg? The only evidence so far is a study by Kazui S et al(Stroke 1996:27:1783-7) showing that SBP > 220mmHg was directly related to haematoma enlargement. The American Heart Association recommends 140mmHg. I stick to 140 as my goal for SBP in spontaneous intracerebral haemorrhage. If I get 140-160mmHg i’m happy. If I go below 140, I know that studies have shown no harm. I try to not have fluctuations, but keep it steady. It is also important to monitor the patient as the SBP is lowered. Some patients with chronic hypertension will have a right shift in their auto regulation curve and lowering their SBP may produce neurological symptoms. They should have a higher SBP titrated. Which antihypertensive to use? Remember that the SBP increases due to an increase in systemic vascular resistance (SVR):
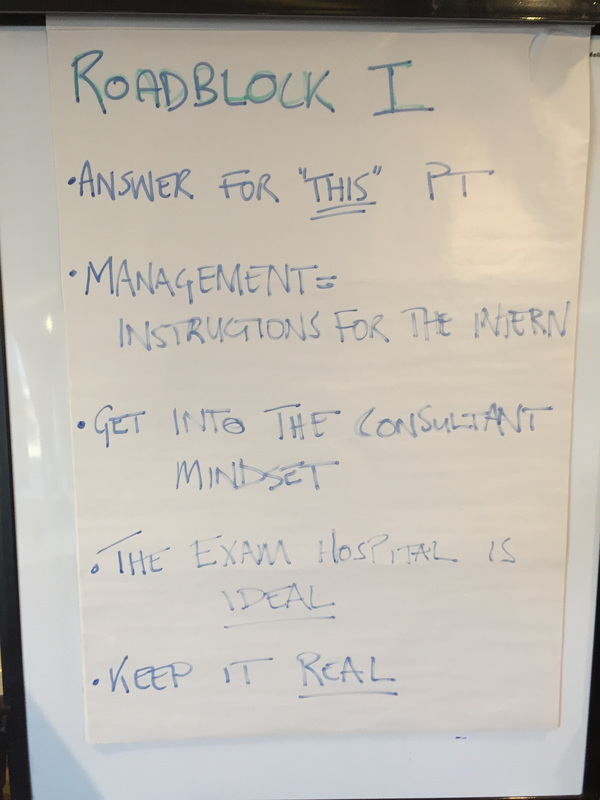
Peter Kas From the RESUS Blog We really enjoyed our second face to face in Melbourne a week or so ago. A big focus was on understanding the exam, and unlocking the questions. More on this in the next blog. We also took the chance to revisit the ABG, and were struck again (as we always are) by the importance of context. Take the following ABG for example.... "a different list of differentials would need to be presented, even thought the acid-base findings might be the same" A few things generally about this exam Its a thinkers exam, so you need to be rested enough to think. Remembering is the order of the day: Follow these simple rules:
THE MCQ ITSELF People put together rules etc. I find that these don't work. I have 4 rules for the MCQ
Good Luck
At fellowshipexam.com we've spent a lot of time on ABGs. They remain one of the most feared and poorly understood props used in the fellowship exam. So we were thrilled when one of our candidates had the confidence to ask a really hard question on the VSG. Keep reading for the question and the commentary. '....a derivation of a derivation using small margins....' |
TAKE ME TO THE COURSE PORTAL!
The fellowship facultyWe work as emergency physicians, and teach, blog and write at resus.com.au Archives
July 2017
Categories |
 RSS Feed
RSS Feed